Surprise Medical Bills: What They Are and How to Avoid Them

Ever opened a medical bill and felt shocked by the amount?
You’re not alone—and it may not be your fault. This is what’s called a surprise medical bill.
At CareSounds, we help patients understand and prevent unexpected charges that can throw off your budget. Here’s what you need to know:
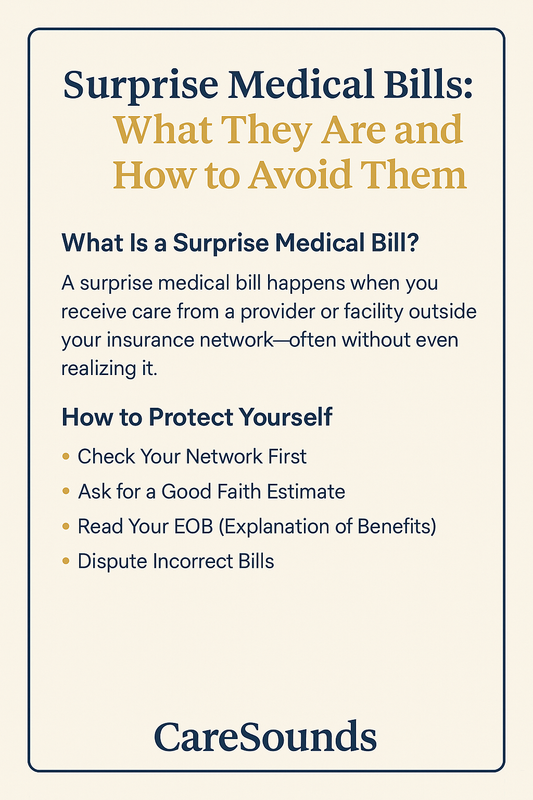
What Is a Surprise Medical Bill?
A surprise medical bill happens when you receive care from a provider or facility outside your insurance network—often without even realizing it. This can happen:
-
During an emergency
-
When a specialist (like an anesthesiologist) isn’t in-network, even if the hospital is
-
When lab tests or imaging are sent to an out-of-network provider
What Changed With the No Surprises Act?
The No Surprises Act, which took effect in 2022, protects patients from many surprise bills—but not all.
It applies to:
-
Emergency care at out-of-network hospitals
-
Non-emergency care at in-network facilities where you're unknowingly treated by an out-of-network provider
However, it doesn’t cover every scenario. That’s where awareness—and support from experts like CareSounds—comes in.
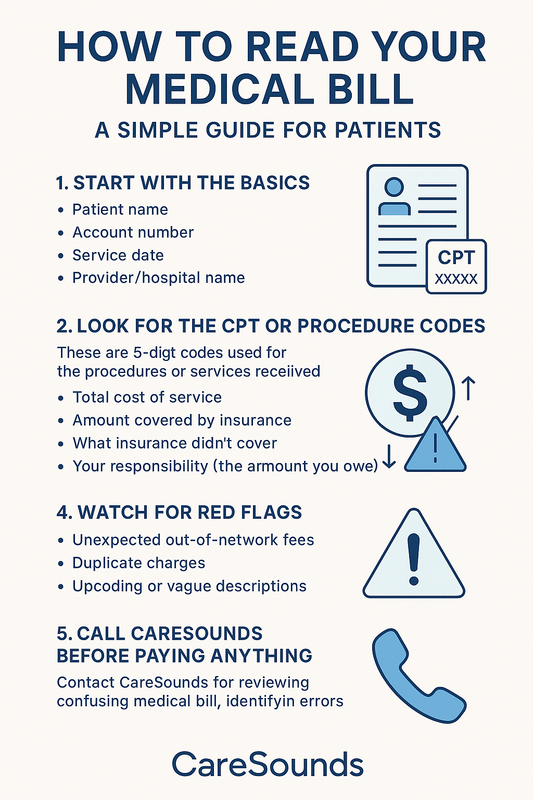
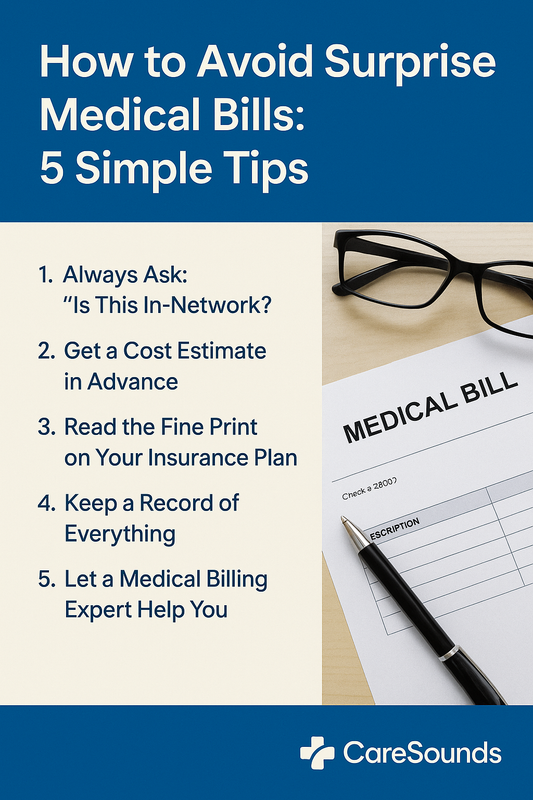
How to Protect Yourself
-
Check Your Network First
Before scheduling appointments or procedures, double-check that everyone involved is in your insurance network—not just the hospital. -
Ask for a Good Faith Estimate
If you’re uninsured or paying out of pocket, you can request a written cost estimate in advance. Providers are legally required to give you one. -
Read Your EOB (Explanation of Benefits)
Don’t ignore this document. It tells you what your insurance covered—and what you may owe. -
Dispute Incorrect Bills
If you think you've been wrongly billed, you can dispute it. And guess what? CareSounds can handle that for you.
How CareSounds Helps You
We review your bills, talk to providers and insurers on your behalf, and fight unfair charges—so you don’t have to.
Whether it’s a surprise bill, coding error, or unclear charge, our billing experts are here to support you.